Organized tracking offers several advantages. It helps demonstrate compliance with privacy regulations like HIPAA, reduces the risk of errors or delays in fulfilling requests, and provides valuable data for auditing and reporting purposes. A well-maintained tracking process streamlines workflows, improves response times, and enhances overall operational efficiency in managing health information exchange.
This foundation of organized record-keeping enables a deeper exploration of topics such as implementing effective tracking systems, best practices for maintaining patient confidentiality, and navigating legal and regulatory requirements related to medical record requests.
Key Components of a Medical Records Request Tracking System
Effective management of health information requests necessitates a structured approach. Several key data points must be consistently logged to ensure comprehensive tracking and facilitate efficient processing.
1: Requester Information: This includes the full name, contact information, and affiliation (if applicable) of the individual or entity requesting the records.
2: Date of Request: Precisely recording the date the request was received is crucial for tracking timelines and managing response deadlines.
3: Description of Records Requested: Detailed documentation of the specific records requested, including dates of service, types of documents, and any other relevant identifiers, is essential for accurate retrieval.
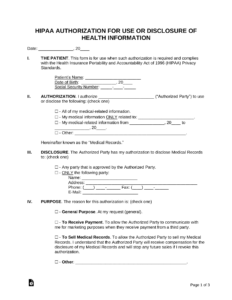
4: Authorization Verification: Confirmation of the requester’s legal authority to access the requested information must be documented. This may involve verifying signed consent forms or other legal documentation.
5: Date of Fulfillment/Denial: The date the request was fulfilled or denied should be recorded for performance monitoring and reporting.
6: Reason for Denial (if applicable): If a request is denied, a clear and concise explanation of the reason, citing relevant regulations or policies, must be documented.
7: Method of Release: Documentation of how the records were released (e.g., electronic transfer, physical copies, fax) helps ensure proper handling and tracking of sensitive information.
8: Recipient Information (if applicable): If the records are released to a third party, their information should be recorded for accountability.
Maintaining these data points facilitates efficient information management, ensures regulatory compliance, and supports a robust audit trail for all medical records requests.
How to Create a Medical Records Request Tracking System
Establishing a robust system for managing requests for health information involves several key steps. A standardized approach ensures consistent data collection and facilitates efficient processing and retrieval.
1: Choose a Format: Select a format suitable for the organization’s needs. Options include spreadsheet software, dedicated database applications, or specialized health information management software. The chosen format should allow for easy data entry, sorting, and reporting.
2: Design the Template: Create a template incorporating the key data points mentioned previously: requester information, date of request, description of records requested, authorization verification, date of fulfillment/denial, reason for denial (if applicable), method of release, and recipient information (if applicable). Clear labels and consistent formatting enhance readability and data integrity.
3: Establish Procedures: Develop clear procedures for staff to follow when receiving, processing, and fulfilling requests. This includes protocols for verifying requester authorization, retrieving records, and documenting all actions taken.
4: Training: Provide thorough training to all staff involved in the process to ensure consistent application of the established procedures and accurate data entry. Regular refresher training reinforces best practices and addresses any updates to regulations or internal policies.
5: Regular Audits: Conduct periodic audits of the system to ensure accuracy, completeness, and compliance with relevant regulations. Audits help identify areas for improvement and maintain the integrity of the tracking system.
6: Secure Storage: Ensure the log, whether electronic or physical, is stored securely to protect patient confidentiality and comply with privacy regulations. Access should be restricted to authorized personnel only.
7: Review and Update: Regularly review and update the template and procedures as needed to reflect changes in regulations, organizational policies, or best practices. This ensures the system remains effective and compliant.
A well-designed system, coupled with consistent procedures and regular review, strengthens compliance, improves efficiency, and protects patient privacy in managing sensitive health information requests.
Maintaining meticulous records of health information requests is not merely a recommended practice, but a critical component of responsible information governance in healthcare and related fields. A standardized system ensures accountability, streamlines workflows, and supports compliance with stringent privacy regulations. From facilitating timely access to information to safeguarding patient confidentiality, a well-designed tracking process provides a crucial framework for managing the complex landscape of health information exchange.
The effective handling of sensitive health data requires constant vigilance and adaptation. Embracing robust tracking mechanisms, coupled with ongoing staff training and adherence to best practices, is essential for navigating evolving regulatory requirements and upholding the highest standards of patient privacy. Organizations must prioritize the development and maintenance of robust systems to ensure the responsible and secure management of protected health information, now and in the future.